President Donald Trump goals to reshape the federal authorities partially by dramatically chopping spending. Well being care is an interesting goal for cost-cutting as a result of it accounts for about 30 p.c of the federal funds.
America spent greater than $1.8 trillion on Medicare, Medicaid, and different well being packages in 2023. The funds deficit was $1.7 trillion that 12 months.
Medicaid alone accounts for $616 billion in federal spending, or 8 p.c of the federal funds.
Medicaid is a federal and state program offering well being protection for about 80 million low-income People. States function this system with oversight from the federal authorities, which reimburses states for a sure proportion of the quantity spent for every beneficiary.
In 2022 the full value of this system was $804 billion. States paid 29 p.c of that quantity, making it the biggest single expense for all states.
As federal funds negotiations are actually underway, some lawmakers have hinted at adjustments to Medicaid, akin to inserting a cap on the quantity reimbursed per particular person, chopping the speed of reimbursement to states, or including work necessities for some beneficiaries.
In the meantime, Trump has mentioned there can be no alterations to Medicaid—or Medicare and Social Safety—besides to root out fraud.
So how a lot fraud, waste, and abuse exists within the Medicaid program?
It’s troublesome to find out as a result of a lot fraud goes undetected.
Primarily based on knowledge from the Authorities Accountability Workplace (GAO) and the Workplace of Administration and Price range (OMB), it seems that lower than 3 p.c of the estimated complete of fraudulent funds are confirmed by a judicial verdict. Some suspected circumstances are resolved by out-of-court settlements, however a lot fraud seems to go undetected.
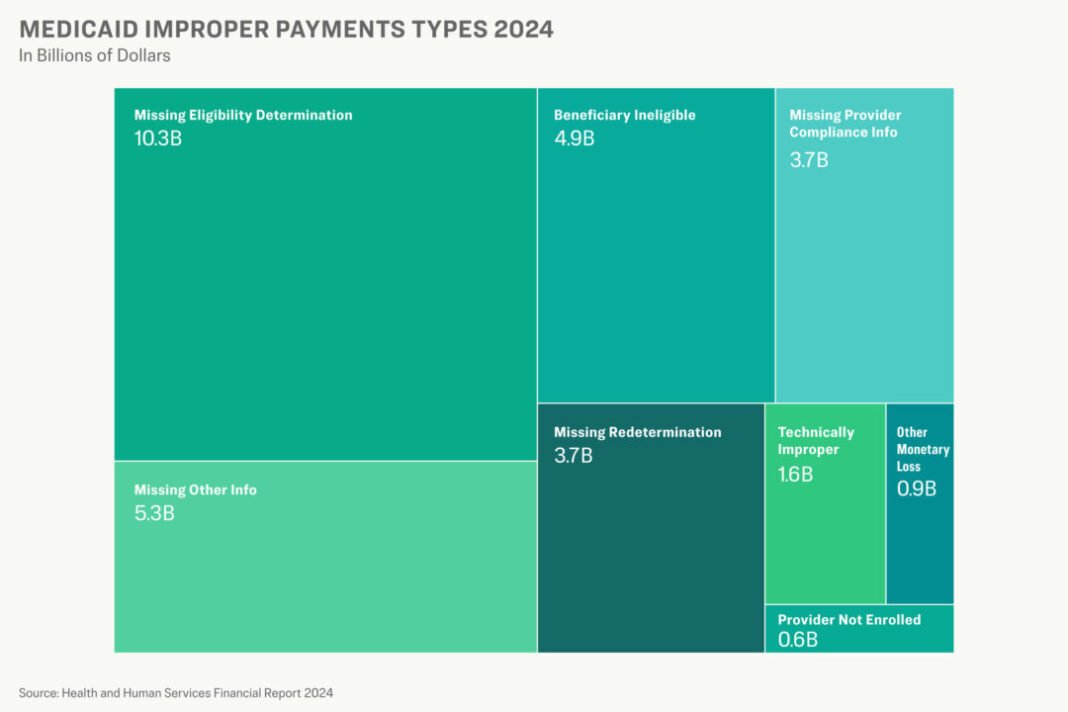
Past fraud, Medicaid loses billions by means of improper funds every year. In 2024, Medicaid made improper funds totaling greater than $31 billion {dollars}, the Division of Well being and Human Providers (HHS) reported.
Most of these funds resulted from clerical errors. Nonetheless improper funds embrace all forms of inaccurate funds, together with fraud, abusive billing, and waste.
The Epoch Occasions examined knowledge on fraud and improper funds within the Medicaid program and interviewed a number of present and former workers members together with the heads of Medicaid Fraud Management Models throughout the nation.
They spoke on the situation of anonymity, as they weren’t licensed to talk to the media, about how fraud and abuse impression this system and the low-income sufferers in want of medical care.
We discovered concerning the extent of the issue, how a lot it might be costing, and the way it hurts the individuals who need assistance probably the most.
Fraud
In Medicaid, as with all federal cost methods, fraud is a truth of life.
“No space of the federal authorities is resistant to fraud,” a GAO report on the topic states. “We estimated that the federal authorities might lose between $233 billion and $521 billion yearly to fraud.”
An OMB report signifies a mean lack of $6.5 billion to fraud over the past eight years, however that features solely confirmed circumstances decided by a court docket. It doesn’t embrace suspected circumstances or circumstances settled out of court docket.
Given the extensive hole between confirmed and estimated losses, it’s troublesome to find out the quantity of precise fraud in Medicaid or any authorities program.
But it exists.
States implement fraud circumstances throughout a wide range of supplier sorts, together with medical doctors, psychological well being professionals, and suppliers of laboratory providers, dwelling care, sturdy medical gear, and long-term care.
Billing for providers not rendered could also be the commonest sort of fraud, sources advised The Epoch Occasions.
One state misplaced an estimated $2 billion to Medicaid fraud over the past 5 years, a workers member in that state’s legal professional normal’s workplace advised The Epoch Occasions.
“They have been preying on people who have been in want of behavioral well being providers,” the workers member advised The Epoch Occasions.
The alleged perpetrators have been luring individuals to stay in substandard circumstances and billing Medicaid for remedies. “They have been, actually, offering them with alcohol and a spot to stay, however not a lot else,” the staffer mentioned. Comparable schemes, typically preying upon homeless individuals, have been perpetrated in different states.
Prescription drug kickback schemes are additionally frequent.
Mississippi, together with 37 different states and Puerto Rico, reached a settlement in an alleged kickback scheme involving Biohaven Pharmaceutical Holding Firm Ltd., a completely owned subsidiary of Pfizer, Inc.
Pfizer agreed to pay $59.7 million, plus curiosity, to settle allegations that Biohaven submitted false claims to Medicaid and different federal packages by providing money and different inducements to well being care suppliers.
4 pharmacists acquired jail sentences for his or her function in a global scheme to invoice Medicaid and Medicare for pharmaceuticals that have been by no means delivered. The fraud resulted in a lack of $13 million.
Hospice fraud is one other frequent scheme, The Epoch Occasions has discovered. Sufferers are enrolled in a hospice program with out their information. When the profit runs out, the affected person’s billing is moved to a different “hospice” owned by the identical supplier.
Residential amenities akin to nursing properties might commit fraud by accepting Medicaid funds however offering insufficient look after Medicaid sufferers.
A Louisiana firm proudly owning 9 nursing properties in 4 states agreed to a $750,000 settlement with the federal authorities and Maryland in 2014 to get rid of expenses that it billed Medicaid and Medicare for “materially substandard and/or nugatory expert nursing facility providers.”
In Mississippi alone, the legal professional normal’s workplace acquired 8,541 complaints associated to abuse, neglect, and exploitation of Medicaid recipients in 2024, a spokesperson advised The Epoch Occasions.
Improper Funds
In 2024, Medicaid made improper funds totaling greater than $31 billion {dollars}, the Division of Well being and Human Providers (HHS) reported. That features overpayments, underpayments, and circumstances by which it’s not identified if the declare was payable.
About 74 p.c of these funds lacked the required documentation, such because the supplier’s Nationwide Supplier Identifier or a sign that the affected person had been recertified for eligibility after one 12 months.
But greater than $5 billion was paid for providers that the sufferers weren’t eligible for or to suppliers who usually are not enrolled within the Medicaid system.
The Epoch Occasions requested clarification from the Facilities for Medicare and Medicaid Providers (CMS) on the share of 2024 improper funds that have been decided to be payable primarily based on the later submission of required documentation. No response was acquired by the point of publication.
The speed of improper funds dropped to five p.c in 2024, down from 8.6 p.c in 2023 and considerably decrease than a excessive of practically 22 p.c in 2021.
The charges from 2020 to 2023 have been affected by a COVID-era waiver of the requirement that the eligibility of every Medicaid affected person be redetermined yearly. State compliance with program necessities additionally improved in 2024, based on CMS.
The federal authorities made greater than $161 billion in improper funds in 2024, of which greater than $7 billion have been confirmed circumstances of fraud, based on knowledge from the OMB.
Obstacles
Medicaid Fraud Management Models recovered $1.2 billion in 2023, which made a return of $3.35 for each greenback spent, based on the Workplace of Inspector Normal (OIG). Investigators say they might do far more if extra assets have been out there.
The dearth of manpower hampers each detection and investigation. Most businesses rely closely on suggestions, complaints, and referrals from different authorities businesses to uncover circumstances of fraud. Some investigative models have in-house knowledge analysts or use knowledge providers from different state businesses to detect fraudulent billing.
As soon as recognized, investigators should prioritize which circumstances to pursue as a result of restricted assets. Some circumstances are pursued as civil circumstances both by the Medicaid Fraud Management Models or different state businesses. Which will end in overpayment restoration however doesn’t embrace felony expenses.
The prosecution of fraud circumstances is usually hampered by an absence of assets, insiders advised The Epoch Occasions. Medicaid Fraud Management Models and district attorneys have restricted assets and the circumstances, whether or not civil or felony, are advanced. Giant for-profit corporations are sometimes in a position to outspend the federal government when defending expenses.
The complexity of the system can be a barrier to detecting fraud.
“Healthcare is so enormous, and billing for it’s such a labyrinthine nightmare, that discovering the dangerous guys is type of like discovering a needle in a haystack,” Neal Okay. Shah, CEO of Counterforce Well being, an organization specializing in medical health insurance claims decision, advised The Epoch Occasions.
Investigators describe catching fraudsters as a sport of Whac-a-Mole. After they shut down one fraud scheme, one other takes its place.
Most improper Medicaid funds—these not essentially triggered by fraud or abuse—outcome from an error by a state worker or contractor. These errors sometimes outcome from excessive turnover of state workers, lack of coaching, or inadequate laptop system edits to deleted eligibility, based on CMS. State investigators additionally say outdated laptop methods utilized in making well being funds make it harder to make appropriate funds and analyze knowledge.
All of that creates a vulnerability, based on insiders, who say their efforts at deterring fraud will solely be as profitable because the system itself. When fraudulent billing seems to be straightforward, suppliers are tempted to abuse the system searching for a payday.
The Medicaid program suffers from fraud and waste, however the actual victims are the beneficiaries.
Insiders advised The Epoch Occasions tales of aged individuals residing in ache after having their medicines stolen, homeless individuals housed in squalid circumstances billed to Medicaid as medical therapy, and aged individuals having their identities stolen for the submission of fraudulent claims.
“You’re defending authorities funds, however you’re additionally defending the individuals who depend on the care to be supplied,” an legal professional working for a state Medicaid Fraud Management Unit advised The Epoch Occasions.
No matter any congressional motion, the president intends to enhance this system, based on White Home deputy press secretary Kush Desai.
“The Trump administration is dedicated to defending Medicaid whereas slashing the waste, fraud, and abuse inside the program—reforms that can enhance effectivity and enhance look after beneficiaries,” Desai advised The Epoch Occasions by electronic mail.
The Epoch Occasions requested feedback from the OIG and OMB however none have been acquired by the point of publication.